By Alyce Collins
THIS LUNG TRANSPLANT recipient has seen her life drastically improve after battling cystic fibrosis since she was only FOUR MONTHS OLD, but she wants to show that just because she’s got new lungs doesn’t mean she’s FIXED after contracting a virus from her donor.
Rima Manomaitis (29) from Massachusetts, USA, was diagnosed with cystic fibrosis at just four months old after her parents noticed she was struggling to gain weight.
Rima lives with cystic fibrosis, gastrointestinal reflux disease, pancreatic insufficiency, chronic sinusitis and cystic fibrosis related arthritis. When she was growing up, Rima didn’t think anything of her condition because she knew no different. Each day, she did two nebuliser treatments, took pills both morning and evening, then lung function tests every few months.

Due to the constant coughing and the strain it required to breathe, Rima couldn’t gain weight, so in 2007 she had a G-tube fitted to provide her with the equivalent of 1,500 calories overnight.
In 2009, while studying, Rima’s lung function was at just 30 per cent, however, she stabled her condition and moved in with her parents after graduating. Although, in 2015 Rima became incredibly sick and required an oxygen machine at all times.
After struggling to get accepted for a double lung transplant despite her failing condition, Rima moved to Minneapolis with her sister, Laima. The transplant centre in Minneapolis listed Rima and she then waited eight months until she received her new lungs via medical organ transportation.

On May 14, 2017, Rima received her double lung transplant from a donor. Rima no longer spends hours every day doing treatments, she isn’t coughing incessantly, nor does she need to take naps each day as she once did. However, Rima’s donor had a dormant virus known as CMV, causing complications in Rima’s recovery. As positive as a transplant is, it doesn’t mean Rima is ‘fixed’ and no longer faces difficulty.
“I was diagnosed with cystic fibrosis when I was four months old,” said Rima.
“They did a sweat test to determine whether I had cystic fibrosis after my parents noticed that I wasn’t gaining weight.
“I think to my parents it was shock. I was too young to realise what it was or what was going on, so my parents were in charge of all my cystic fibrosis stuff. I grew up thinking it was normal.

“I had to do nebuliser treatments twice a day, get manual PT which is when someone uses their hands and hits you on the upper and lower back, sides, upper and lower chest. This is to break up the sticky mucus that’s in the lungs all the time. It helps break up the mucus so it’s easier to cough up.
“In the years leading up to my transplant, my breathing treatment were increased so I was doing four nebulized treatments in the morning and evening and several more throughout the day, to open up my airways more.
“I was also on IV antibiotics for ten months before getting my new lungs to stable me enough until I got the call.
“I also have to take pills in the morning and evening as well as enzymes every time I ate anything. This is because I’m pancreatic insufficient, meaning my pancreas can’t produce them itself.
“Along with all that, I had to go to my cystic fibrosis clinic every few months to do lung function tests and to make sure everything was okay.
“I first found out that I may need a double lung transplant in the winter of 2009. My lung function was down to 30 per cent and that’s usually when doctors consider it.

“I stayed stable for a few years, hovering in the mid-twenties for lung function until 2012. This is when they became more serious about getting me evaluated for one. It wasn’t a rush, so I was able to complete all the tests and appointments over a period of a few months.
“Once all that was done, they decided I was ‘too well’ at the time, but I was a good candidate. So they wanted to monitor me by seeing me every six months.
“It was in 2015 that I became very sick and needed oxygen and they said I really needed to get listed. At this point my sister had decided to become my carer and was going to move from Brooklyn to come help me.
“She found a good transplant centre in Minneapolis and after all the testing in the spring of 2016, they decided I would be a good candidate and would do my transplant. That following September, after being sick all summer, Laima and I moved, and I was listed shortly after getting there.
“In that time, I had two dry runs, which is when I got the call to say there was a donor, but then the operation was cancelled because there ended up being an issue with the donor lungs.
The transplant wasn’t without its complications because her donor had CMV, a virus which can remain dormant until it becomes active. For transplant recipients, CMV can result in organ rejection.

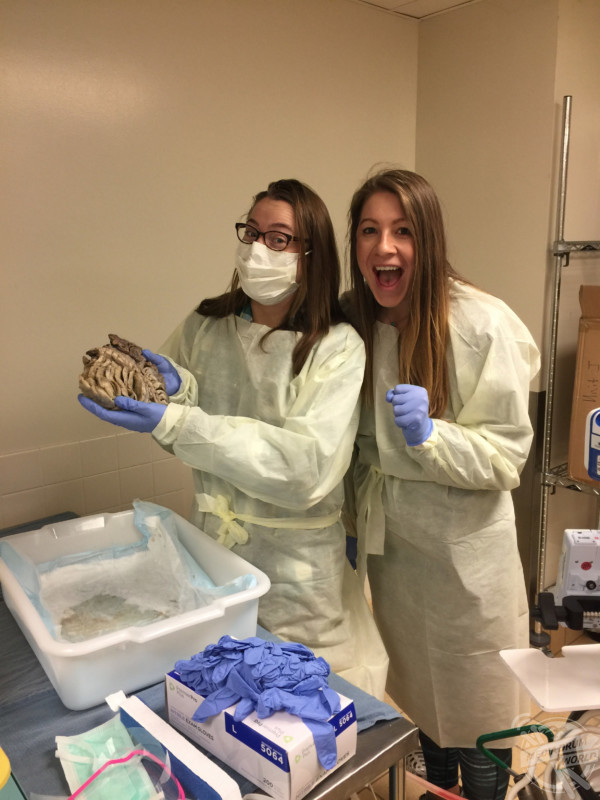
Although her life has improved drastically, Rima still faces health difficulties each day as she will take anti-rejection medication for the rest of her life and may need another transplant in the future. Rima still wears a face mask around children or in polluted areas because there’s still a risk of getting sick while in public.
“My recovery was pretty quick. The first year is usually the most important because that’s when most things go wrong,” said Rima.
“It takes a while for your body to get used to the change and all the new medicines that you’ll be on for the rest of your life. A handful of issues surely popped up. My white blood cell levels were all over the place.
“My donor had CMV, which I didn’t have but I have now. CMV is a virus that’s usually dormant in people and isn’t contagious. For someone who is immunocompromised, such as me, it can cause problems.
“The main issue is that it can cause rejection. Last spring, my body was still adjusting to medicines and my haemoglobin and white blood cell count were so low that I ended up in the hospital for a week and needed a blood transfusion.
“Since the transplant, my life has changed tremendously. I don’t have to spend hours a day doing treatments. I’m not coughing all day or taking naps every day, I’m no longer on IV antibiotics either.
“I can now walk, carry things, do the laundry, clean the house and climb stairs without needing to stop to catch my breath or to have a cough attack. I’m able to live my life.
“All I need to do now is take pills twice a day and get labs once a week to monitor my levels, as well as see my transplant team every three months.
“I want people to know that a transplant isn’t forever. Just because I got a transplant, doesn’t mean I’m ‘fixed’ forever. They can last anywhere from a year to 20 years. Rejection is a real thing.
“I still have to worry about getting sick when I’m in public. I wear a mask in most shops when they’re busy, on public transport or in a crowd indoors. I also wear a mask when the air quality is bad.
“I generally stay away from children because they are petri dishes full of germs. Being immunocompromised, I can get sick very easily, and clearly, I’ve become a slight germaphobe.
“Cystic fibrosis is an end stage disease. With more awareness comes funding for research to develop life changing therapies and medications. I’m sick of seeing my friends and people I know suffering and dying. I have high hopes that a cure will be found soon.”
To see more, visit www.instagram.com/lung_story_short






