By Alyce Collins
THIS TWENTY-ONE-YEAR-OLD was given paracetamol and sent home after doctors thought she had tonsillitis due to her MOUTH ULCERS but she was admitted to hospital THE VERY NEXT DAY with a rare bone marrow failure that required FIFTY BLOOD TRANSFUSIONS – and doctors said if she hadn’t gone to hospital when she did she wouldn’t have survived another day.
Admin assistant, Annie Lovegrove (21) from Ipswich, UK, developed a mouth ulcer in January 2019 and after trying to get rid of it with saltwater, she went to her GP for antibiotics.
Antibiotics were prescribed for a week, but Annie didn’t notice any progress, so she went back to her doctor, as she’d developed a temperature of 41 degrees Celsius. She was then diagnosed with tonsillitis and given paracetamol as the doctor noticed sores on her tonsils.

The following day, Annie’s temperature was soaring, and her heart rate became erratic so Annie’s mother, Hayley (48) saw her daughter’s state spiralling and trusted her mother’s intuition and called an ambulance.
As soon as she arrived at the hospital on January 26, Annie’s blood pressure was taken and was found to be very low. Initial blood tests showed that Annie’s platelet count was just three and her neutrophils were 0.01. Annie was classed as neutropenic as she had a severely low count of white blood cells and neutrophils in her blood, putting her at risk of infection.
For the first two weeks in hospital, Annie was in and out of sleep throughout the day, with a fever over 42 degrees. She had to be placed in isolation because she couldn’t risk infection, and anything could be a health threat.
In February, Annie was diagnosed with severe aplastic anaemia, a rare bone marrow failure which causes a lack of blood cells in the body. Since her admission to hospital, Annie has had over 50 blood transfusions, consisting of 50 pints of blood, and 70 bags of platelets.

“I had a mouth ulcer form in the middle of January, along with unexplained bruises on my body,” said Annie.
“After a week of using over the counter medication and saltwater, my mum told me to go to the doctor as there was no improvement. If anything, it was getting worse.
“I was prescribed antibiotics, but I started to feel unwell with headaches and a lack of energy. After a week it still wasn’t getting any better, so my mum took me back to the GP. The second time, they diagnosed me with tonsillitis because I had developed sores on my tonsils.
“My temperature was 41 degrees and I was prescribed more antibiotics as well as paracetamol. The doctor told my mum that if it wasn’t any better in a couple of days, she should call 111.
“However, the next day my temperature was getting worse and my pulse was sporadic. Thankfully, my mum called an ambulance right away because she knew there was something seriously wrong.
“When we got to hospital, they immediately ran blood tests and checked my blood pressure. Tests showed that my haemoglobin level measured 45, but a healthy count would be around 15. My platelet count was just three and my neutrophils were 0.01. This is when they realised just how sick I was.
“I had to have three pints of blood and platelets transfused within 24 hours of arriving. Then over the next two weeks in hospital, I received five more pints of blood and four pints of platelets. This basically kept me alive.
“I was in and out of sleep continuously because I was so weak– I didn’t use my phone for two weeks because I was that bad. I was in isolation as I was neutropenic, and I couldn’t risk getting infections since everything was a risk to me.
“Initially, my family were told that it could be leukaemia and they were devastated, understandably, but, my first bone marrow biopsy in February confirmed that it was aplastic anaemia, which left us with a sense of relief at first.
“However, once we read into it and learned more about the condition, we soon realised that leukaemia may have been less challenging to treat because aplastic anaemia is such a rare form of bone marrow failure. Only two people in every million are diagnosed with it a year.
“There are different classifications of it, and as my neutrophils were 0.01, I was classed as very severe aplastic anaemia.”

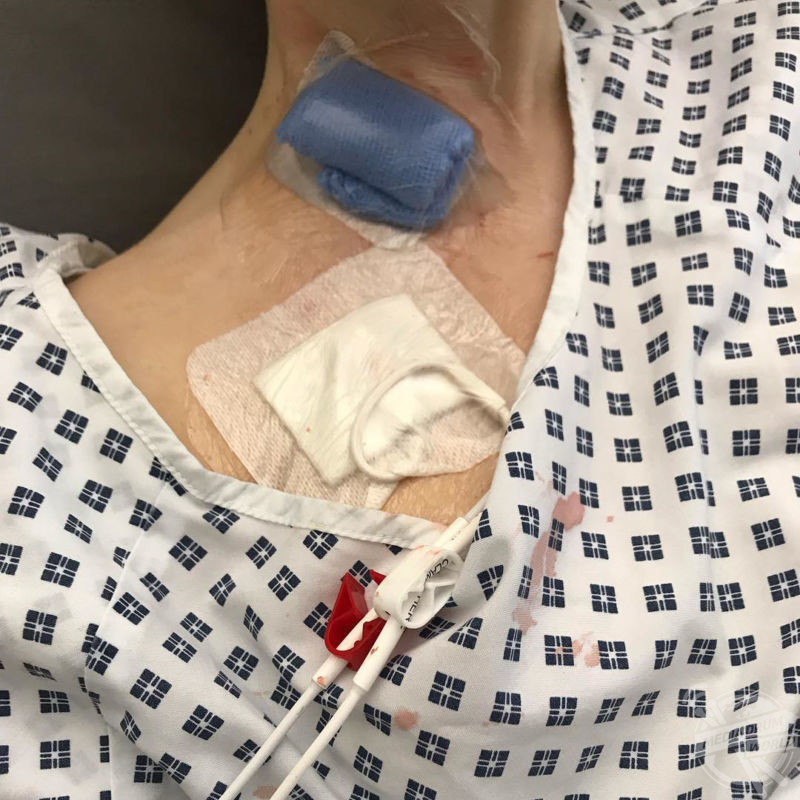
A bone marrow transplant was the best form of treatment for Annie, but before this could happen, she had to endure high dosage chemotherapy to reset her immune system and bone marrow before receiving the donor stem cells.
On May 17, Annie received a bone marrow transplant from her younger sister, Millie (17), who was a good match. Annie will undergo tests to ensure that she doesn’t reject the transplant over the coming year.
“I lost my hair due to the aggressive chemotherapy I had to have to reset my body ready for the transplant. For a 21-year-old, that was quite devastating, but I’m learning to live with it,” said Annie.
“I also had to undergo egg preservation as the chemotherapy may have made me infertile. That was a gruelling process, especially while going through the effects of aplastic anaemia simultaneously. I harvested 15 eggs, which are frozen and ready for whenever I want to start a family.
“My little sister, Millie, was a good match luckily and she donated her stem cells on May 15 and 16, and they were then transplanted to me in an IV drip on May 17.
“It’s hoped that I won’t reject the transplanted stem cells within the first year because that gives me a much better chance at beating this condition. I’d still need monitoring annually and lots of blood tests in the future though.

“Since my diagnosis, I haven’t been able to see many people other than my immediate family because the risk from catching a common cold could be fatal. I’m hoping that once my blood levels improve, I’ll be able to start leading a normal life again.
“This year has been a write off because every time I get a high temperature of more than 37.5 degrees, we have to contact the hospital and I have to be admitted so they can check my infection markers and put me on antibiotics.
“I get very fatigued and need to rest a lot. Everyday routines take much longer and I require assistance from my mum. It’s also made me paranoid about germs and the chance of catching an infection, so I’m constantly aware of what I eat, drink and touch.
“It’s important that people don’t ignore the signs, like bruises and ulcers because that was my body’s way of telling me it was deteriorating. If we didn’t go to A&E when we did, doctors said I wouldn’t have survived the next day.
“The whole journey has been traumatic for myself and my family, who have been with me through every step of the journey.
“People ask me how I’ve got through it all, but I’ve just taken each day as it comes and trusted the medical team supporting me.”
To see more, go to www.instagram.com/anniesstory2019 or donate to www.justgiving.com/crowdfunding/anniesstory?utm_id=108&utm_term=pmVPymgp7






